News
The Chemistry of Sleep
By: Miranda Wood and Melissa Leyden, UVA ChemSciComm
Looking at sleep from a chemical perspective reveals its intricate yet fundamental role in maintaining our health. Research continually uncovers more about how biological functions are regulated by the amount of sleep we get. So far, these studies have revealed much about how closely linked sleep is to the release of specific chemicals in various brain regions, and how these processes play a crucial part in our overall well-being and cognitive function.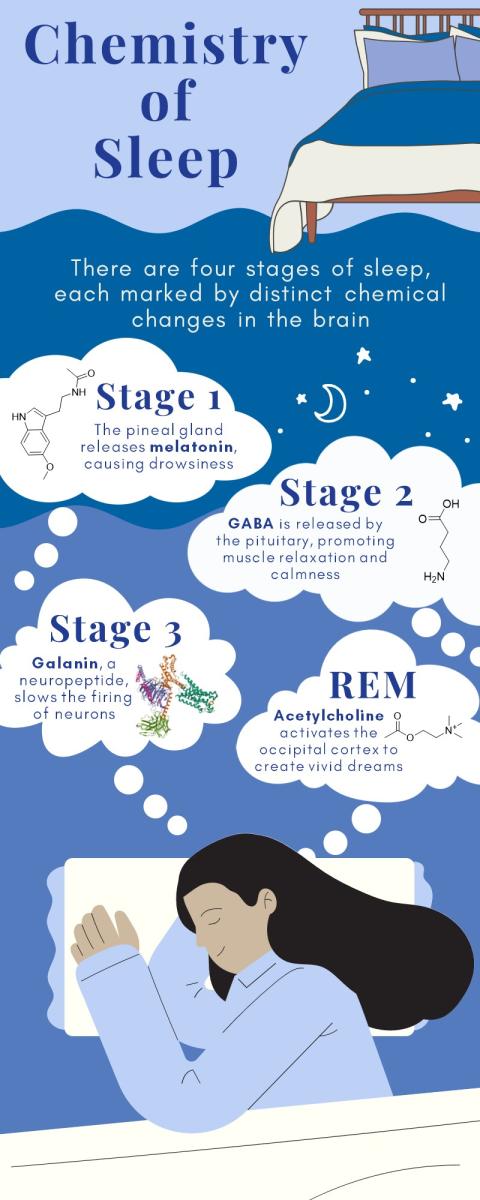
Sleep unfolds through distinct stages, each marked by unique chemical and physiological changes in the brain. During the day, adenosine, a byproduct of metabolic and neuronal activity, accumulates in the brain during wakefulness, signaling how long we've been awake.1 It directly inhibits wake-promoting regions in the hypothalamus, causing us to become drowsier the longer we’re awake. Once in bed, Stage 1, lasting several minutes, ushers us into light sleep, where natural movements slow, and muscles relax.2 Melatonin, an indoleamine hormone, is produced by the pineal gland and released at night as a response to light signals from the retina.3 This hormone helps regulate our circadian rhythms and sleep-wake patterns, but is particularly important in the first phase of the sleep cycle. Stage 2, the longest portion of the sleep cycle, involves increased muscle relaxation and slowed brain wave activity, occasionally punctuated by bursts of electrical activity.2 γ-Aminobutyric acid, or GABA, an inhibitory neurotransmitter, helps soothe brain activity and promotes muscle relaxation in this stage of sleep.4 Stage 3, a deep, restorative sleep phase, exhibits the slowest breathing, brain waves, and heart rate.2 These non-REM stages are heavily influenced by chemicals like GABA and galanin, a neuropeptide chemical messenger that reduces the firing of neurons.5
As we progress through the sleep cycle, we reach REM (rapid eye movement) sleep, occurring approximately 90 minutes after falling asleep.2 During REM sleep, our eyes move rapidly behind closed lids, and brain waves become mixed in frequency. Heart rate and breathing turn irregular, and this is the prime time for vivid dreaming. Acetylcholine, released from REM-on cells in the pons, takes center stage, activating brain regions responsible for visual processing (such as the occipital cortex) and crafting vivid dreams.6
Waking up involves the activation of various neurochemical nuclei, with dopamine, acetylcholine, histamine, serotonin, and norepinephrine playing key roles.7 These neurochemicals form extensive neuronal networks that support our daily wakefulness. Acetylcholine generates swift brain waves to rouse us, while norepinephrine boosts our brain's alertness.6,7 Serotonin cells help regulate body temperature and wakefulness, with SSRI medications prolonging serotonin's action in synapses.7 Histamine also plays a significant role in wakefulness, and dopamine contributes to alertness and cognitive function. These meticulously orchestrated sleep cycles and neurochemical processes ensure we experience both restorative sleep and wakefulness.
Insomnia, characterized by persistent difficulty falling asleep or staying asleep, involves complex chemistry. Neurotransmitters like norepinephrine and epinephrine play significant roles in insomnia by keeping the brain in a heightened state of alertness, increasing activity, and preventing the onset of sleep.8 Additionally, cortisol, a hormone released from the brain to the body's hypothalamic-pituitary-adrenal (HPA) axis, can exacerbate insomnia, especially during stressful times or in the morning when cortisol levels peak naturally.9 Another factor contributing to insomnia is orexin (also known as hypocretin), a wake-promoting neuropeptide that ensures we don't fall asleep when we shouldn't, further complicating the chemistry of sleep and adding to the challenges faced by those with insomnia.9
Our mental and physical well-being heavily relies on balanced sleep cycles and rest. The biochemical processes that impact sleep are intricate and rely on many different chemical factors. Understanding what each hormone, protein, and molecule controls can be used to understand sleep disorders and patterns to improve our overall health. To counteract the negative effects of poor sleep and improve your overall sleep quality, consider implementing the following general recommendations: maintain a consistent sleep schedule by going to bed and wake up at the same time every day, even on weekends, to regulate your body's release of sleep-related hormones. Additionally, getting exposure to natural daylight during the day and limiting blue-light exposure at night can balance your circadian and improve overall sleep quality.
References
1.Bjorness, T. E.; Greene, R. W. Adenosine and Sleep. Current Neuropharmacology 2009, 7 (3), 238–245. https://doi.org/10.2174/157015909789152182.
2.Gottesmann, C. GABA Mechanisms and Sleep. Neuroscience 2002, 111 (2), 231–239. https://doi.org/10.1016/s0306-4522(02)00034-9.
3.Srinivasan, V.; Spence, W. D.; Pandi-Perumal, S. R.; Zakharia, R.; Bhatnagar, K. P.; Brzezinski, A. Melatonin and Human Reproduction: Shedding Light on the Darkness Hormone. Gynecological Endocrinology 2009, 25 (12), 779–785. https://doi.org/10.3109/09513590903159649.
4. Tillage, R. P.; Sciolino, N. R.; Plummer, N. W.; Lustberg, D.; L Cameron Liles; Hsiang, M.; Powell, J. M.; Smith, K. G.; Jensen, P.; Weinshenker, D. Elimination of Galanin Synthesis in Noradrenergic Neurons Reduces Galanin in Select Brain Areas and Promotes Active Coping Behaviors. Brain Structure & Function 2020, 225 (2), 785–803. https://doi.org/10.1007/s00429-020-02035-4.
5.Watson, C. J.; Baghdoyan, H. A.; Lydic, R. Neuropharmacology of Sleep and Wakefulness. Sleep Medicine Clinics 2010, 5 (4), 513–528. https://doi.org/10.1016/j.jsmc.2010.08.003.
6.Sateia, M. J.; Buysse, D. J.; Krystal, A. D.; Neubauer, D. N.; Heald, J. L. Clinical Practice Guideline for the Pharmacologic Treatment of Chronic Insomnia in Adults: An American Academy of Sleep Medicine Clinical Practice Guideline. Journal of Clinical Sleep Medicine 2019, 13 (02), 307–349. https://doi.org/10.5664/jcsm.6470.
7.Irwin, M.; Clark, C.; Kennedy, B.; Christian Gillin, J.; Ziegler, M. Nocturnal Catecholamines and Immune Function in Insomniacs, Depressed Patients, and Control Subjects. Brain, Behavior, and Immunity 2003, 17 (5), 365–372. https://doi.org/10.1016/s0889-1591(03)00031-x.
8.Ban, H.J.; Kim, S. C.; Seo, J.; Kang, H.-B.; Choi, J. K. Genetic and Metabolic Characterization of Insomnia. PLoS ONE 2011, 6 (4), e18455. https://doi.org/10.1371/journal.pone.0018455
9.Mogavero, M. P.; Silvani, A.; Lanza, G.; DelRosso, L. M.; Ferini-Strambi, L.; Ferri, R. Targeting Orexin Receptors for the Treatment of Insomnia: From Physiological Mechanisms to Current Clinical Evidence and Recommendations. Nature and Science of Sleep 2023, Volume 15, 17–38. https://doi.org/10.2147/nss.s201994.
